T1D and Health: How Long Will You Live?
Glycemic control is not as good of a predictor as metabolic fitness is.
Listen to this really fun AI-generated audio summary of this article.
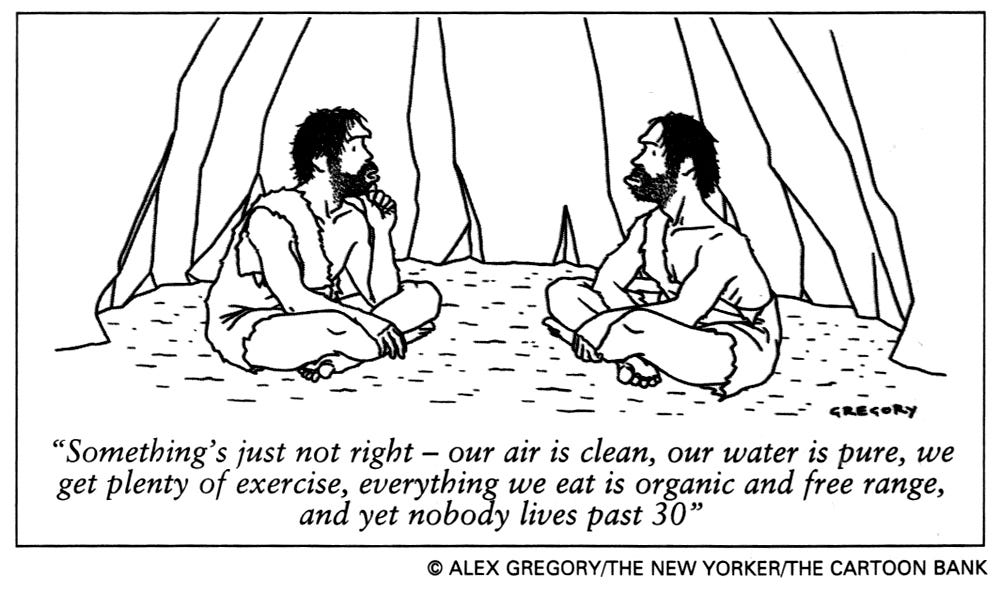
As medical research tells us, all we need to live long, healthy lives are having clean air and water, eating well, and getting lots of exercise. So, why do some says that prehistoric people only lived to be around 30 when their conditions couldn’t have been better?
Primarily because it’s funny. But it’s also a myth. Anthropologists actually say that the average age of prehistoric people was more like 32-ish, but many lived well into their 70s and 80s, much like we do today. The lower average was due to premature death from things like childbirth, infections and getting eaten by lions.
As for diabetics, especially those of us with type 1 diabetes (T1D), most literature says that we generally live about 12-15 years less than the population at large, but like the cartoon, these are gross estimates of averages, which is now an average of averages. This doesn’t tell you very much, or provide any prescription for extending your life.
Rather than try to evaluate your lifespan, it’s more meaningful to evaluate your various risks of all-cause mortality by engaging more in things that reduce overall risk, while avoiding things that increase risk. In this context, we’re only talking about things that we can control—that is, our daily lifestyle choices.
Fortunately, we don’t need to worry about being eaten by lions anymore. In fact, the state of California reports that the number of people killed by lions has dropped to only 1.5 per year since 1986! Good for us, sad for the lions.
These days, the biggest modifiable risk factor under our personal control is elevated glucose levels, which is true among all humans, not just those with diabetes.
Well, that and smoking.
In fact, we’ll show studies later that illustrate how the “hazard ratio” between smoking and diabetes is roughly equal. We all know that (and how) smoking can cause all sorts of health problems, but so does elevated glucose levels, leading to cardiovascular disease, kidney and liver disease, hypertension, and many other factors.
Of course, we T1Ds already know this, so what’s new here?
The trap that T1Ds get into is the belief that attaining “target” or “ideal” glucose levels is itself “healthy.” Well, yes, but only by comparison to dying prematurely if your glucose levels are higher. This is like saying that smokers can live longer if they quit or reduce their level of smoking. Again, yes, but only by way of not dying earlier. If you quit smoking—or achieve non-diabetic glucose levels—you just bring your life expectancy back to baseline, where your risk profile is governed by your metabolic fitness, which has always been the largest factor anyway. While reducing risk is good, your real goal should be to add to your lifespan beyond the averages by engaging in activities that improve your metabolic fitness.
T1Ds may hear that and feel overwhelmed: “It’s hard enough just to reduce glucose levels, but you also expect me to improve other things too? At the same time? You’re crazy!”
No, actually, I’m not, and neither are the researchers who’ve found that, ironically, by focusing on improving metabolic health, you will consequently improve glucose control far more easily and with considerably less effort than if you tried other interventions (like diets and drugs). More importantly—and surprisingly—this research also finds that improved metabolic health can add to longevity, despite glucose levels not reaching targets.
A much better way to view this is by looking at the different ways there are to reach target glucose levels. There’s low-carb diets, there’s super-tight insulin control, and there’s exercise. (In the future, there will also be drugs like GLP-1 agonists and others in that domain, but that’s a different topic altogether, as the evidence is not yet clear on the effect these interventions will have on metabolic health, separately from glucose control.)
If one is to aim for lower glucose levels and improving metabolic health, we can easily infer that exercise will achieve both. Is it “easier” than carb restriction? Many believe it is, but there’s also evidence to show that carb-restricted diets not only don’t help in metabolic fitness, but can exacerbate the problem by introducing other comorbidities, even if they are successful in reducing overall glucose levels. (I’ll be writing about this in a separate article.)
Let’s begin by looking at studies that measure the effects of exercise among those who have and don’t have diabetes.
The health benefits of “metabolic fitness”
In 2018, Mandsager and colleagues studied more than 122,007 adults between 1991 and 2015, with a median follow-up of 8.4 years, and published their findings in the article, “Association of Cardiorespiratory Fitness With Long-term Mortality Among Adults Undergoing Exercise Treadmill Testing.” They found that the more physically fit people were (as measured by treadmill testing), the longer their lifespan, even in the presence of other comorbidities, such as hypertension, coronary artery disease, or even smoking and diabetes. In fact, the positive effects from good metabolic fitness were so disproportionate after factoring in these comorbidities, they found there was no greater predictor and protector of all cause mortality than cardiovascular fitness.
The following chart illustrates the beneficial effects as measured by “hazard ratio,” which is defined as a weighting for how much more likely you are to die: The higher the number, the greater the risk. Note that Diabetes (1.4) is roughly equal to smoking (1.41). (ESRD is end stage renal disease, or kidney failure.)
The section labeled “Group comparison” shows the risk of all-cause mortality is greatest when the cardio fitness is low (vs elite) by five orders of magnitude. As fitness levels improve, the benefit tapers off relative to the previous fitness level, but it still has a much larger aggregate effect on overall health risk than any of the comorbidities in the cohort.
Consider the “Adjusted HR” value for “Low vs. Below Average.” The difference between these two (from a fitness level) is the difference between sitting around all day and taking a 15-minute walk once or twice a day, preferably after meals. That’s right, just a simple walk can improve your lifespan by several years (not to mention quality of life), according to the paper, “Walking for Exercise,” from Harvard’s School for Public Health.
Of course, the faster or longer you walk, the greater the benefit, as the increased activity improves your metabolic fitness. As you ratchet up the hazard ratio ladder, you reduce your risk for all-cause mortality, in spite of confounding factors, like smoking and diabetes.
To see how metabolic fitness directly affects T1Ds, Larry Distiller (Principle Physician and Managing Director at the Centre For Diabetes And Endocrinology in Johannesburg) conducted a comprehensive literature review called, “Why do some patients with type 1 diabetes live so long?” where he cites multiple studies that all come to similar conclusions.
All the people in the dozens of studies he reviewed were shown to have excellent cardiovascular health, despite having elevated glucose levels. One article included in his review is the “Golden Years Cohort,” which includes 400 T1Ds who’ve had the disease for over 50 years. Their mean HbA1c was 7.6% (± 1.4), with some levels as high as 8.5%-9%. None had an HbA1c below 7%. Interestingly, among those who happened to die early had significant problems with lipids (high cholesterol), kidney disease, and other factors, any of which could be exacerbated by high glucose levels, but the correlation was weaker. That is, they showed signs of significant metabolic stress independently of A1c levels.
This comports with the data shown in the chart earlier: One’s hazard ratio is highest when cardio fitness levels are the lowest, while the hazard ratio is lowest for those with the elite cardio fitness levels, all independent of other comorbidities.
Cardio Fitness as part of the T1D self-management protocol
As a result of these and other studies, treatment in people living with T1D is beginning to shift towards improving overall metabolic health in parallel to attaining lower glucose levels. One example is this article about how Belgium is focusing primarily on metabolic health, with glucose control as a secondary goal.
Imagine that: glucose control as a secondary goal.
The best way to improve cardiovascular health is aerobic exercise, but there are also other interventions, such as lipid-lowering therapies (statins), antihypertensive therapy (to lower blood pressure), adjunct therapies such as metformin, sodium–glucose transport protein 2 (SGLT2) inhibitors and glucagon-like peptide-1 receptor (GLP1) agonists. These are just now coming into focus in T1D managed care, and more time is needed to determine optimal dosing strategies as to assess long-term complications (if any).
But, let’s be clear: No other intervention has more metabolic health benefit than exercise, especially for T1Ds.
An article published in the October, 2024, issue of Diabetes Care titled, “Sitting Time and Its Interaction With Physical Activity in Relation to All-Cause and Heart Disease Mortality in U.S. Adults With Diabetes,” author Sandra S. Albrecht from Columbia University found that “longer sitting time was associated with greater all-cause and heart disease mortality risk in inactive or insufficiently active adults with diabetes, but not in active adults.”
Note, in Albrecht’s study, she defines “inactive” as moderate to vigorous physical activity less than 10 hours per week, whereas “active” is defined as greater than 150 hours per week. But one doesn’t have to go wild and sweat all day in pursuit of exercise. Albrecht found that merely standing is better than sitting, walking is better than standing, and running/jogging/cycling/elliptical trainers is better than walking. The more you do, the better your health outcomes, independently of other factors.
Yes, It’s a spectrum, but the benefits are not linear—they’re more logarithmic. That is, the benefits are greatest going from nothing to something, and diminishes from there. For example, walking achieves a huge benefit after eating any meal at all, yielding vastly improved glucose clearance, insulin efficacy and sensitivity. As you increase activity, metabolic fitness improves, but the benefits spread out more generally throughout the body.
Alas, exercise is hard, particularly for T1Ds who don’t own lions. Exercise affects insulin dosing, which is difficult for those who use pumps and automated (closed-loop) delivery systems (because algorithms can’t really know how much to adjust insulin delivery, especially in real-time). First, the user needs to tell the system they’re about to exercise, which is challenging enough, but what the system chooses to do is subject to error. Most T1Ds experience dramatic hypoglycemia, leading to their just giving up on serious exercise.
T1Ds who manage themselves using multiple daily injections (MDI) also find it hard, but studies show that such users tend to be more personally engaged with their disease, so their learning curve to new situations tends to be quicker and more successful.
Either way—MDI or AID systems—T1Ds still need to learn how to manage glucose levels for exercise, and teaching that is highly individualized. Clinicians don’t have the time, let alone the training, to design such protocols on an individualized basis.
In the paper published in the British Journal of Medicine titled, “Attitudes and barriers to exercise in adults with a recent diagnosis of type 1 diabetes: a qualitative study of participants in the Exercise for Type 1 Diabetes (EXTOD) study,” T1Ds were interviewed about their experiences with exercise since their diagnosis, and the primary detractors were fear of hypoglycemia, and lack of encouragement to exercise by their doctors (with some saying their doctors recommended against exercise to avoid hypoglycemia).
That doesn’t mean T1Ds are doomed—quite the opposite. In the paper, “How we do it”: A qualitative study of strategies for adopting an exercise routine while living with type 1 diabetes,” researchers surveyed T1Ds who exercise effectively and summarize their findings:
“Living an active lifestyle with T1D is facilitated by dedicated structure and organization of routines, accepting the need for trial and error to understand the personalized glycemic responses to physical activity and careful use of food to prevent hypoglycemia. These themes could inform clinical practice guidelines or future trials that include PA interventions.”
As someone who exercises a lot myself, I can affirm this is what I went through as well. Everyone’s experience varies, but (as I conclude at the end of this article), the best way to start is simply by walking after every meal.
Albrecht would be proud of you. Send her a note of thanks.
With that background, let’s review what mitochondria is and its relationship to T1D.
It’s the metabolism, baby
The basic biology of life requires converting fuel into energy in order to make things happen, such as growing cells, repairing tissues, fighting diseases, and the basic function of thought. No matter what happens in the body, energy must be created, and that’s all done by these tiny little organelles called mitochondria, which has been termed the engine that makes life happen. The more mitochondria you have, the more energy you can create. And more efficient each cell is, the better your body is at utilizing fuel. Put these two together and you have a way to measure “metabolic fitness.”
If you have high cholesterol, your metabolic fitness affects how well your body recovers from the atherosclerosis in your arteries. If you have cancer, your metabolic fitness will affect how well your immune system fights it off. If you’re running away from lions, your metabolic fitness governs how well your muscles will move to escape danger. If you have high glucose levels, your metabolic fitness will affect how well your body can tolerate and recover from these insults. If you have a brain, your metabolic fitness will somehow enable you to better understand this article.
So integral is mitochondria to the function of the body that improving your metabolic fitness effectively reduces your risk of all-cause mortality across the board, even in the presence of other risk factors, including T1D, thereby extending life beyond population-wide averages.
While drugs are great for treating conditions that arise in life, such as taking statins to lower cholesterol levels, or taking insulin to reduce glucose levels, these interventions are treating symptoms—they’re not directly affecting the holistic metabolic system. If you have underlying metabolic dysfunctions, or even metabolic inefficiencies, your body can suffer all sorts of health problems that may be independent of diabetes, further raising your risk profile.
Naturally, you want to lower glucose levels, and while insulin can do this, it’s not the only way to do so. Exercise also reduces glucose levels, but that’s where things get tricky. Let’s start with insulin.
The pros and cons of insulin therapy
Insulin helps mediate the process in which cells absorb glucose, but it, like glucose, is best when there is not too much, and not too little. Too little insulin is obvious: we die. Too much insulin causes hypoglycemia, which is also bad, as it can feel as dreadful as being eaten by a lion.
While the “right” amount of insulin necessary to keep glucose levels in ideal ranges seems like it should be our goal, using only insulin to manage glucose levels is too simplistic. This was an unexpected lesson learned from the Diabetes Complicates and Control Trial (DCCT) conducted between 1985 and 1994.
In the 1980s, there was a dispute in the medical community as to whether sustained elevated glucose levels (hyperglycemia) in T1Ds was responsible for a series of microvascular complications, such as retinopathy (leading to blindness), kidney disease, and neuropathy. Some felt there was a causal relationship, whereas others felt these were byproducts of a more general (genetic) condition inherent to the disease. Six years into the trial, it was pretty clear that these complications were, in fact, due to hyperglycemia. T1Ds who were on more aggressive insulin regimens to keep glucose levels lower experienced fewer of these microvascular complications. So, the recommended standard of care was to increase insulin dosing to reduce glucose levels, and has remained that way since.
Unfortunately, it took a while before the data was scrutinized more carefully to observe that other complications with intensive insulin treatment affected the study group. In the 2014 article in Diabetes Care, The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study at 30 Years: Overview, the authors found that, while those who were under tighter control didn’t suffer microvascular damage as much, there was an increase of macrovascular damage, including cardiovascular disease (CVD), leading to heart attacks and strokes, among other comorbidities.
To understand this relationship between intensive insulin treatment and “metabolic health,” we focus on the fact that insulin will convert excess glucose into each of six different types of fat. (Yes, insulin is the only way to create fat in the body; thus, the relationship between weight and insulin levels—not calories—is usually in parity.)
Of particular interest is visceral fat, a particular type that wraps around vital organs, such as the heart, liver, kidneys, and intestines. Visceral fat not only interferes with these organs’ primary functions, but it also interferes with insulin-mediated glucose absorption, one of a variety of forms of insulin resistance, which is one form (or indicator) of metabolic syndrome. In this case, “lipid-induced insulin resistance.”
When caloric consumption exceeds energy expenditure (i.e., eating more than exercising), excess glucose in the bloodstream is not absorbed by muscle tissue, so instead, it’s stored as fat, and insulin is the sole mechanism for that.
In a non-diabetic whose beta cells are still functional, the pancreas will make more insulin, whereas, a T1D who cannot produce insulin injects it (using an insulin pen or a pump). Either way, when insulin converts excess glucose into fat, it adds to the visceral fat that was already present. Because that visceral fat is a source of insulin resistance, progressively more insulin is needed to overcome that resistance in order to clear that glucose from the bloodstream. That added insulin makes more fat, increasing the resistance. It’s just a pile-on effect.
As calories and insulin continue, the feedback loop accelerates: the greater the insulin resistance, the greater the need for more insulin, which creates more visceral fat, feeding back into the loop.
For the non-diabetic, the demand from more insulin puts increasing stress on the beta cells where, at some point, they fail to produce enough insulin to clear circulating blood glucose. That’s when daily blood glucose levels start to rise, and with it, A1c levels—5.5% to 6% to 6.5% and higher. This is the point where a T2D diagnosis is made, even though the actual onset of diabetes began years earlier.
Making matters worse, many T2Ds now act like T1Ds and inject the insulin that their bodies can’t make enough of. By just adding more insulin, they’re not only failing to address the problem—metabolic syndrome—but are actually making it worse.
I mention all that about T2Ds because T1Ds suffer the same problems for the same reasons, and we are seeing this metabolic disorder today. In a meta-analysis titled, “Obesity in Type 1 Diabetes: Pathophysiology, Clinical Impact, and Mechanisms,” the researchers noted that Obesity in adults with T1D rose from 3.4% at baseline (1986 to 1988, before the DCCT) to 22.7% in 2004 to 2007, after the DCCT recommendations encouraged tighter control using intensive insulin therapy. The most recent data, according to the Lancet article, “Obesity in people living with type 1 diabetes,” show that T1D obesity reached 37% in 2023, with a corresponding increase in cardiovascular events and all-cause mortality.
T1Ds, just like T2Ds, can be well on their way towards obesity, but are only getting started, and are making matters worse by taking increasingly more insulin with the well-intended aim of keeping glucose out of the bloodstream.
This is a snow-plowing effect: Rather than remove the snow, we just push it further and further into a bigger pile. Sure, sidewalk may be clear of snow, much like the bloodstream may be clear of glucose, but the snow (and glucose) is still there, building up, creating more damage. The sidewalk may be clear, but we can’t get into the house.
We think of the pancreas as the center of glucose regulation, but it’s the metabolic system that plays a far more integral part in the causes and effects of glycemic activity. Aiming for perfect glycemic control is not, by itself, optimizing risk factors, and the very attempt at doing so (via more insulin) may make things worse.
Metabolic fitness as both a predictor and a protector of all-cause mortality
Every single bodily function is so dependent on our metabolic system for efficient energy management, that mitochondrial fitness is both the primary predictor of all health outcomes, and the primary protector against the deleterious effects from various assaults on our bodies.
For example, a study from 2022 titled, “Cardiorespiratory Fitness and Mortality Risk Across the Spectra of Age, Race, and Sex,” involved 750,302 U.S. veterans aged 30 to 95 for a median of 10 years. The authors found that the most metabolically fit individuals had a lower risk profile for all-cause mortality, even among those who have other comorbidities, including hypertension, diabetes, coronary artery disease, cancer, and even smoking.
The least fit group in this cohort—those at or below the 20th percentile—had a more than four-fold increase in risk of all-cause mortality compared to those in the extremely fit group (≥98th percentile), a trend which also persisted across stratifications by race and sex.
It should be no surprise that all of these stats are applicable to T1Ds. In fact, researchers who’ve studied mortality rates and causes among T1Ds consolidated their findings into the literature review paper I cited earlier, “Why do some patients with type 1 diabetes live so long?” The authors conclusions comport with the Cardiorespiratory Fitness study cited above, and for the sake of clarity, I will repeat the two key points from the paper that I cited earlier:
“It is apparent that good glycaemic control alone cannot explain why some patients with type 1 diabetes avoid fatal CVD events,” and “one of the major factors linked with long-term survival is the absence of features of metabolic syndrome.”
Putting this in practical terms for T1D health risks, let’s consider two scenarios.
If you are metabolically unfit—that is, in the lower 20th percentile—and you also have excellent glucose control, your risk of all-cause mortality is still quite high, because your risk of dying from other (non-T1D) incidents is high, just as if you were one of the non-diabetics in the cardiorespiratory study.
If you are metabolically fit—that is, the upper 80th percentile, which implies that you’re getting roughly 10-15 hours a week of intensive exercise—your risk of all-cause mortality is reduced considerably, even if your glucose levels are modestly elevated over time, just as was determined in the Cardiorespiratory Fitness study. Here, a healthy metabolism allows your body to recover from not just illnesses, but damage caused by higher glucose levels, not too differently than recovering from other, non-diabetes related factors (for example, high cholesterol).
At the risk of sounding stupidly obvious and patronizing, exercise yields healthier metabolic fitness, which lowers your risk of all-cause mortality, even if your T1D is not tightly controlled.
Now, it also happens that exercise lowers glucose and cholesterol levels, which eases both the act and the stress of T1D management, so your T1D will more likely be under good control as a side-effect.
How to measure metabolic fitness
Metabolic fitness is measured using a metric called, V02max, which represents the maximum (max) volume (V) of oxygen (02) that a person can utilize during intense exercise. It has become such an accurate measure of metabolic fitness, that it is now used in virtually all studies that aim to evaluate risk of all-cause mortality.
There are many ways to measure your V02max, but the easiest is the 1-mile walk test, which has been validated against the gold standard lab test that’s extremely difficult and expensive to perform. You can use a smartwatch or heart rate monitor to measure your heart rate as you walk one mile as fast as you can (without running or jogging). When you’re done, measure (or observe) your heart rate 10 seconds after completion, and then input this data into this form (which also explains details of how/why this test works). Your V02max results will be normalized for your age and gender, and a chart on that page will tell you your fitness level. It’s a pretty basic formula, so you can find the forms everywhere online.
As you increase exercise levels, remember that your mitochondria is adaptive. It spins up or slows down in response to the physical activity, albeit slowly over time (again, with variability among individuals). Accordingly, your insulin requirements are going to change, which requires getting used to.
Taking too much insulin makes it very hard to exercise—in fact, fear of hypoglycemia is the primary reason why most T1Ds don’t exercise. Expect to reduce insulin intake before exercise activities. This is why it’s important to start slowly—by walking, say, 15-20 minutes after meals—and building up to more intensive workouts as your fitness improves and your insulin dosing levels adapt. (More likely than not, your basal insulin rate will be reduced earlier and more.)
Exercise, by way of improved metabolic fitness, will help you reduce your glucose levels and insulin in a healthier way than all other interventions, resulting in lower weight and a reduced risk of many micro- and macrovascular complications. Best of all, you’ll be so healthy that if a lion decides to attack you and your friends, it’ll be just as it was in prehistoric times: You won’t need to outrun the lion, just your friends.





The study showing that cardiovascular fitness is a bigger factor than blood glucose level as expressed in the HbA1c, is Very Big in my estimation. Over many decades as a T1D, I have pursued both exercise and "normal healthy" HbA1cs , so this blog post is valuable to me in setting my goals.
"...if a lion decides to attack you and your friends, it’ll be just as it was in prehistoric times: You won’t need to outrun the lion, just your friends." That's the equivalent of most bike theft prevention strategies: make yours harder to steal than its neighbors.